Balance declines with age, but exercise can help stave off some of the risk of falling

My wife and I were in the grocery store recently when we noticed an older woman reaching above her head for some produce. As she stretched out her hand, she lost her balance and began falling forward. Fortunately, she leaned into her grocery cart, which prevented her from falling to the ground.
Each year, about 1 in every 4 older adults experience a fall. In fact, falls are the leading cause of injuries in adults ages 65 and older. Falls are the most common cause of hip fractures and traumatic brain injuries.
Injuries like those are also risk factors for placement in a nursing home, where the fall risk is nearly three times higher than for people living in the community.
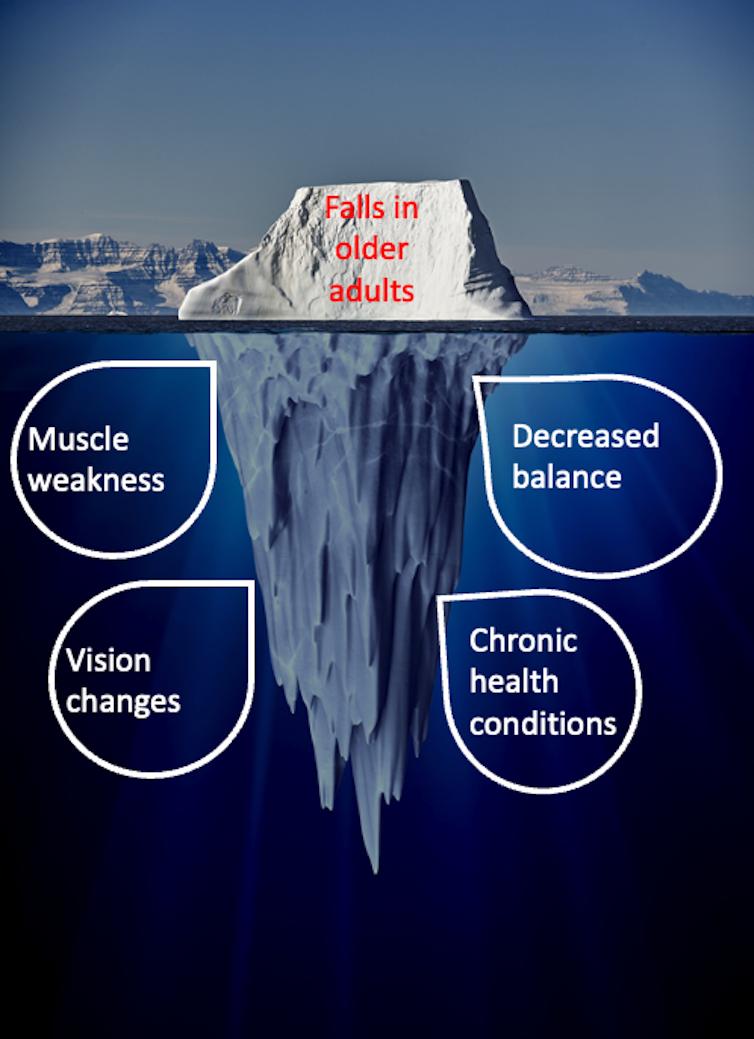
A number of physical changes with aging often go unseen preceding falls, including muscle weakness, decreased balance and changes in vision.
I am a physical therapist and clinical scientist focused on fall prevention in older adults, commonly ages 65 and older. I’ve spent most of my career investigating why older adults fall and working with patients and their families to prevent falls.
Why aging leads to increased risk of falls
Aging is a process that affects the systems and tissues of every person. The rate and magnitude of aging may be different for each person, but overall physical decline is an inevitable part of life. Most people think aging starts in their 60s, but in fact we spend most of our life span undergoing the process of decline, typically beginning in our 30s.
Older adults are more prone to falling for various reasons, including age-related changes in their bodies and vision changes that leave them vulnerable to environmental factors such as curbs, stairs and carpet folds.
Based on my experience, here are some common reasons older adults may experience falls:
First, aging leads to a natural loss of muscle strength and flexibility, making it more challenging to maintain balance and stability. The loss of strength and poor balance are two of the most common causes of falls.
Second, older adults often have chronic conditions such as arthritis, Parkinson’s disease or diabetes that can affect their mobility, coordination and overall stability.
In addition, certain medications commonly taken by older adults, such as sedatives or blood pressure drugs, can cause dizziness, drowsiness or a drop in blood pressure, leading to an increased risk of falls.
Age-related vision changes, such as reduced depth perception and peripheral vision and difficulty in differentiating colors or contrasts, can make it harder to navigate and identify potential hazards. Hazards in the environment, such as uneven surfaces, slippery floors, inadequate lighting, loose rugs or carpets or cluttered pathways, can significantly contribute to falls among older adults.
Older adults who lead a sedentary lifestyle or have limited physical activity may also experience reduced strength, flexibility and balance.
And finally, such conditions as dementia or Alzheimer’s disease can affect judgment, attention and spatial awareness, leading to increased fall risk.
Theories of aging
There are numerous theories about why we age but there is no one unifying notion that explains all the changes in our bodies. A large portion of aging-related decline is caused by our genes, which determine the structure and function of bones, muscle growth and repair and visual depth perception, among other things. But there are also numerous lifestyle-related factors that influence our rate of aging including diet, exercise, stress and exposure to environmental toxins.
A recent advance in scientific understanding of aging is that there is a difference between your chronological age and your biological age. Chronological age is simply the number of years you’ve been on the Earth. Biological age, however, refers to how old your cells and tissues are. It is based on physiological evidence from a blood test and is related to your physical and functional ability. Thus, if you’re healthy and fit, your biological age may be lower than your chronological age. However, the reverse can also be true.
I encourage patients to focus on their biological age because it empowers them to take control over the aging process. We obviously have no control over when we are born. By focusing on the age of our cells, we can avoid long-held beliefs that our bodies are destined to develop cancer, diabetes or other conditions that have historically been tied to how long we live.
And by taking control of diet, exercise, sleep and other lifestyle factors you can actually decrease your biological age and improve your quality of life. As one example, our team’s research has shown that moderate amounts of aerobic exercise can slow down motor decline even when a person begins exercise in the latter half of the life span.
Fall prevention
Adopting lifestyle changes such as regular, long-term exercise can reduce the consequences of aging, including falls and injuries. Following a healthy diet, managing chronic conditions, reviewing medications with health care professionals, maintaining a safe home environment and getting regular vision checkups can also help reduce the risk of falls in older adults.
There are several exercises that physical therapists use to improve balance for patients. It is important to note however, that before starting any exercise program, everyone should consult with a health care professional or a qualified physical therapist to determine the most appropriate exercises for their specific needs. Here are five forms of exercise I commonly recommend to my patients to improve balance:
Balance training can help improve coordination and proprioception, which is the body’s ability to sense where it is in space. By practicing movements that challenge the body’s balance, such as standing on one leg or walking heel-to-toe, the nervous system becomes better at coordinating movement and maintaining balance. A large research study analyzing nearly 8,000 older adults found that balance and functional exercises reduce the rate of falls by 24%.
Strength training exercises involve lifting weights or using resistance bands to increase muscle strength and power. By strengthening the muscles in the legs, hips and core, older adults can improve their ability to maintain balance and stability. Our research has shown that strength training can also lead to improvements in walking speed and a reduction in fall risk.
Tai chi is a gentle martial art that focuses on slow, controlled movements and shifting body weight. Research shows that it can improve balance, strength and flexibility in older adults. Several combined studies in tai chi have demonstrated a 20% reduction in the number of people who experience falls.
Certain yoga poses can enhance balance and stability. Tree pose, warrior pose and mountain pose are examples of poses that can help improve balance. It’s best to practice yoga under the guidance of a qualified instructor who can adapt the poses to individual abilities.
Flexibility training involves stretching the muscles and joints, which can improve range of motion and reduce stiffness. By improving range of motion, older adults can improve their ability to move safely and avoid falls caused by limitations in mobility.
Use of assistive devices can be helpful when strength or balance impairments are present. Research studies involving the evaluation of canes and walkers used by older adults confirm that these devices can improve balance and mobility. Training from a physical or occupational therapist in the proper use of assistive devices is an important part of improving safety.
When I think back about the woman who nearly fell in the grocery store, I wish I could share everything we have learned about healthy aging with her. There’s no way to know if she was already putting these tips into practice, but I’m comforted by the thought that she may have avoided the fall by being in the right place at the right time. After all, she was standing in the produce aisle.![]()
Evan Papa, Associate Professor of Physical Therapy and Rehabilitation Science, Tufts University
This article is republished from The Conversation under a Creative Commons license. Read the original article.