Colorado community mental health centers struggle with Medicaid drop
Click play to listen to this article.
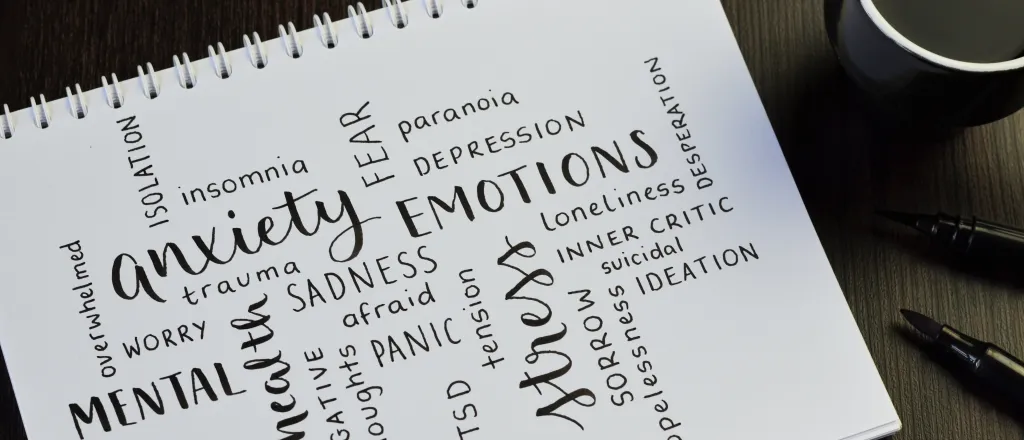
(Colorado News Connection) It's been about a year since the official end of the COVID public health emergency - which has led to a significant drop in Medicaid enrollments and a rise in uninsured individuals in Colorado.
This poses challenges for community mental health centers, like the Jefferson Center for Mental Health, where the rate of Medicaid enrollee decline has surpassed earlier predictions. It has remained below pre-pandemic levels since January.

Dr. Kiara Kuenzler, president and CEO of the Jefferson Center for Mental Health, said it's now facing a daunting $6 million shortfall.
"The people that we're serving are just in extreme stress, struggling to deal with regaining health-care benefits. That impacts not only their access to behavioral health care, but all of their health-care needs," she said.
The nonprofit KFF recognizes the need for behavioral health at an all-time high in its 2023 Colorado fact sheet- identifying more people than ever reporting mental health and substance use challenges.
Kara Johnson-Hufford, Colorado Behavioral Health Care Council CEO, emphasized the urgent need for support for these clinics. She noted a projected shortfall of $24 million to $29 million for these centers overall could mean a risk of reduced services, longer wait times and compromised care.
She added many individuals who have lost Medicaid coverage and now have private insurance are also seeking treatment less frequently - or discontinuing it altogether - due to co-pays and deductibles.
"More people than ever are now going without insurance. No longer qualifying for Medicaid, but cannot afford private insurance - or they may be giving up on Medicaid altogether because of the emotional toll of the enrollment process just being too great," she continued.
Johnson-Hufford predicted if reimbursement mechanisms don't keep pace with the need, programs will close. Despite efforts to address the issue, such as helplines and complaint processes, she said the gap in funding remains a critical concern.