Rapid tests play a crucial role in curbing COVID-19 infections – especially as people gather for the holidays

Nathaniel Hafer, UMass Chan Medical School
As winter begins and the holidays are in full swing, the COVID-19 pandemic has entered another worrying phase. Emergence of the omicron variant, along with increasing rates of infections, have left many people unsure about their holiday plans.
On Dec. 2, 2021, President Joe Biden outlined a series of actions to respond to the COVID-19 pandemic, including making at-home COVID-19 rapid tests eligible for reimbursement by private insurance. Along with vaccination, testing remains one of the most effective ways to track and reduce transmission of SARS-CoV-2, the virus that causes COVID-19.
Even though COVID-19 testing has become part of most people’s everyday conversation, many people still have questions about the difference between antigen and PCR tests, including when and how to use them.
I’m a molecular biologist based at UMass Chan Medical School. Since April 2020, I’ve been part of a team working on a National Institutes of Health-funded program called RADx Tech to help companies develop rapid tests to detect when a person is infected with COVID-19.
How rapid antigen tests work
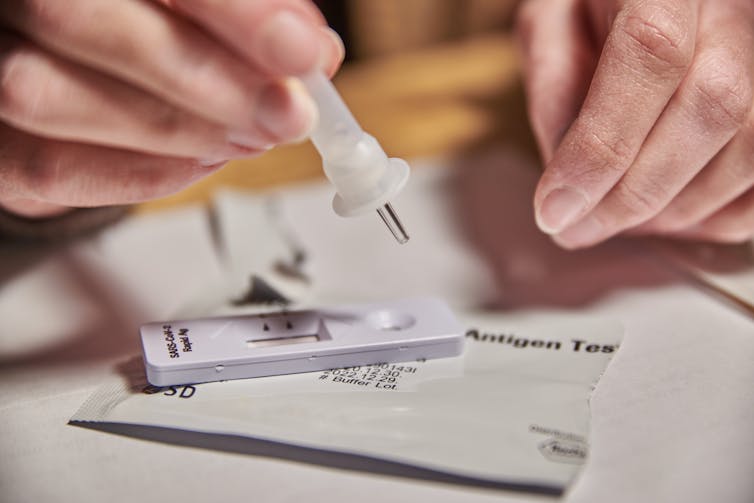
Rapid antigen tests are designed to detect a portion of protein – known as an antigen – of SARS-CoV-2. First, you take a sample from your nose or mouth with a swab, as directed. You mix the sample with liquid that breaks apart the virus. You then apply the liquid to a test strip that has antibodies specific for SARS-CoV-2 painted on it in a thin line. Antibodies are Y-shaped proteins that recognize and bind to foreign substances such as antigens. If the antibodies bind to the virus proteins, or antigens, a colored line appears on the test strip, indicating the presence of SARS-CoV-2.
These tests are convenient because they are easy to use and provide results quickly, typically within about 15 minutes. Another benefit is that antigen tests can be relatively inexpensive, at around US$10-$15 per test. In contrast, PCR tests usually require laboratory equipment and technicians, take 12 hours to several days to get results and cost $100 or more, though there are many ways to get these tests free of charge.
In his announcement, President Biden also discussed plans to distribute 50 million free tests to community health care providers for people without insurance. People should check their local media outlets for information about when free rapid tests become available. In Colorado, free rapid tests have been available to families with school-age children for months. Be prepared to act quickly: In late November, 100,000 people signed up in less than 24 hours for free antigen COVID tests in New Hampshire.

As of early December 2021, the Food and Drug Administration has authorized about a dozen rapid antigen tests for SARS-CoV-2, which means these tests meet certain standards for performance and accuracy.
When to use rapid tests
If you have any symptoms of COVID-19, regardless of whether you’ve been vaccinated, you should get tested right away with either a PCR or antigen test.
SARS-CoV-2 can spread very easily, even if you don’t have symptoms. The faster you can determine if you have COVID-19, the sooner you can isolate yourself, which helps prevent transmission to others. Early testing is also critical because new drugs like those from Merck and Pfizer are most effective if given early in the course of infection, soon after symptoms appear.
If you get a negative antigen test but still feel sick, it is possible that you received a false negative test. Isolate yourself away from others and contact your health care provider to discuss your symptoms. If you get a positive test, you should isolate yourself at home and contact your health care provider as soon as possible.
If you don’t have symptoms but have had close contact with someone with COVID-19, what to do depends on your vaccine status. If you’re fully vaccinated, the CDC currently recommends that you wait five to seven days after your exposure and then get a PCR or rapid antigen test. If you’re not fully vaccinated, get tested right away. If you don’t develop symptoms, you should still get retested five to seven days after your exposure.
Like many respiratory viruses, it takes several days for SARS-CoV-2 to build up in your body after exposure. During this early phase of infection, the amount of viral protein is relatively low, and a rapid test may not detect your infection. This is why serial testing over multiple days, with at least 24 hours between each test, is recommended for many antigen tests. Rapid antigen tests are most often accurate when a person is infectious, because that is when the highest amount of virus is in the respiratory tract.
Studies have shown that serial antigen testing – typically two to three tests in one week – is on par with a single PCR test. Remember that a test is only a snapshot of your SARS-CoV-2 status at the time of the test. It’s possible, especially with antigen tests, to test negative during the early stages of infection.
The future for at-home COVID-19 testing
Despite all that we researchers have learned, there is still more to understand about the best way to use rapid tests. Our team is conducting several studies to fill these gaps.
One question we are studying with a program called STOP COVID-19 is how people use home tests when their infection risk is low versus high. For instance, someone who wears a mask indoors and does not eat out at restaurants may be considered low risk, while someone who is not vaccinated and gathers with many people without masks is considered high risk. We are also interested in knowing whether people will adhere to a testing regimen when they have an exposure, and whether they will share their home test results with their local department of public health.
Another major question our team is studying is: How do antigen tests compare with PCR tests when it comes to detecting COVID-19 in people who are positive but have no symptoms? A separate nationwide study called Test Us at Home is generating important data that will help us answer this question in the next few months.
Rapid antigen tests are a welcome tool in society’s fight against the COVID-19 pandemic. When used properly and in combination with other tools such as vaccination, mask-wearing and good hygiene, these actions can help limit the spread of SARS-CoV-2 this holiday season.
[Like what you’ve read? Want more? Sign up for The Conversation’s daily newsletter.]![]()
Nathaniel Hafer, Assistant Professor of Molecular Medicine, UMass Chan Medical School
This article is republished from The Conversation under a Creative Commons license. Read the original article.