This overdose-reversal medicine could reduce opioid deaths – so why don't more people carry it?

Tarlise Townsend, University of Michigan and Freida Blostein, University of Michigan
Forty-seven thousand Americans died of opioid-related overdoses in 2017 – similar to the number of deaths from car accidents and gun violence.
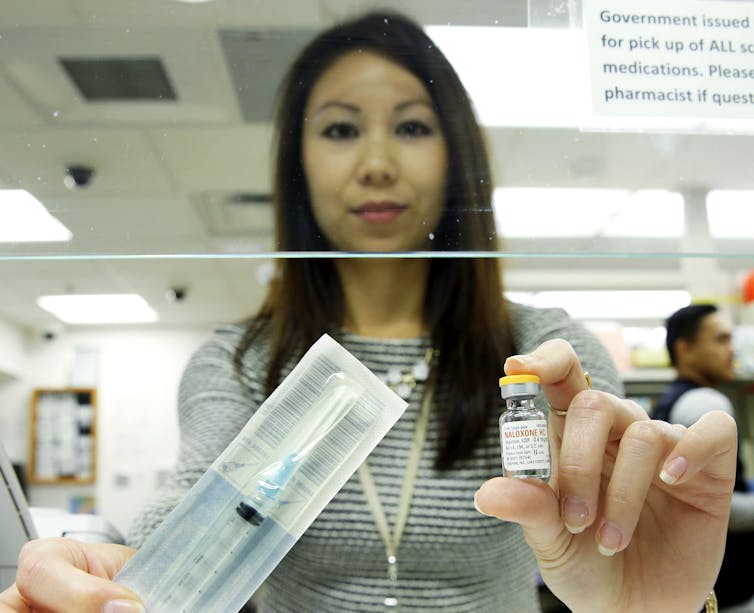
That number could have been much lower had more people received naloxone, a medication that reverses opioid-related overdose.
Naloxone is safe, non-addictive and highly effective. And it does more than save lives: When used shortly after overdose, naloxone reduces the likelihood of long-term brain damage from diminished blood flow.
Available as an injection or nasal spray, naloxone can be administered by anyone trained to do so - assuming, that is, that someone has it on hand at the scene of the overdose.
Restricted access
Police, firefighters and medical first responders are increasingly equipped with naloxone.
However, the true first responders to an overdose often aren’t professionals but the friends, family and peers of people who use heroin and other opioids. Relatively few of these “laypeople” have access to naloxone, which is available via community distribution, a doctor’s prescription or, in states that allow naloxone to be sold without a prescription, from a pharmacy.
While at least 41 states allow pharmacists to dispense the medicine without a prescription, many pharmacies fail to actually stock it. In California, only a quarter of all pharmacies carried naloxone last year.
As opioid-related deaths have soared, there’s been an increase in programs working to get naloxone into the community. Health centers like Prevention Point Pittsburgh, for example, train people likely to witness overdose on how to recognize the signs and give them free naloxone.
However, the most recent available data suggest that relatively few communities with high rates of opioid-related deaths actually have such programs.
Even emergency medical personnel, or EMS, may not have naloxone when they need it.
Most U.S. states only authorize intermediate- and advanced-level EMS to carry and administer the drug. But in many parts of the country – particularly rural and tribal areas – EMS with basic training are often the only medical first responders immediately available in emergencies.
‘Moral hazard’
One impediment to increased naloxone access is the argument that reviving overdose victims will encourage opioid use.
Naloxone critic Dr. Harold Jonas, founder of the website Sober.com, has warned health care providers that naloxone creates a safety net, making people think “they don’t need treatment for substance abuse and … continue using at will.”
The fear that life-saving interventions encourage reckless behavior – a concern historically used to oppose everything from condoms to seat belts – is called “moral hazard.”
There is no peer-reviewed, empirical evidence that naloxone use encourages opioid use. But this argument remains pervasive.
Often, politicians combine moral hazard with budgetary arguments to oppose broader naloxone distribution.
The prices of some naloxone products have been rising. Between 2009 and 2016, naloxone manufactured by Amphastar almost doubled in price, from US$20.34 to $39.60 per dose.
In 2017, the city of Middletown, Ohio, spent almost $35,000 on naloxone administered by EMS in 966 opioid overdose calls – up from $11,000 and 532 calls in 2016.
Citing cost, Middletown Councilmember Dan Picard has said the city should refuse to resuscitate people who overdose repeatedly.
Naloxone is cost-effective
Since the opioid crisis disproportionately hurts low-income communities like Middletown, our team of health policy and epidemiology researchers at the University of Michigan conducted a study to determine whether naloxone is a good use of the scarce resources available to reduce opioid-related deaths.
Our study, published in International Journal of Drug Policy, found that naloxone is extremely cost-effective.
We analyzed the cost-effectiveness of giving naloxone to three different groups: laypeople, police and firefighters and EMS.
When all three groups have naloxone, it costs about $16,000 per year of “high-quality” year of life saved. We accounted for quality of life as well as quantity, since problematic substance use increases the risk of hepatitis, HIV and other illnesses.
As life-saving interventions go, $16,000 per high-quality year of life is an excellent deal. The public defibrillators used to revive people in cardiac arrest come out to around $53,797. And a breakthrough class of new cancer drugs run $100,000 to $150,000 per high-quality year of life saved.
Naloxone actually saves society money when we take the lost economic productivity from fatal overdoses into account, we found. Hard-hit communities may see naloxone as an expense – but they’re actually saving the city money by keeping more of its workforce alive.
This finding holds even when we add in a city’s criminal justice costs associated with opioid use.
Naloxone would remain cost-effective even if the “moral hazard” concerns were true. We found that overdose rates would have to rise 20% for lay distribution of naloxone to cease being cost-effective – a large margin of error for an unsubstantiated worry.

Moral imperative
Our research determined that the most cost-effective strategy is to distribute naloxone to all three groups: laypeople, police and firefighters, and EMS.
If low-income communities can’t afford that much naloxone, however, the next-best scenario is to give the medicine to laypeople plus at least one first responder group – either police and fire or EMS.
Getting naloxone into lay hands is so critical because many overdose witnesses hesitate to call 911 due to fear of arrest, stigma or loss of government benefits like subsidized housing. No matter how many first responders have naloxone, the victims in those cases cannot benefit from it. They need someone close by, like another person using opioids, to revive them.
But emergency responders should have naloxone as well since overdose witnesses may not always have naloxone or be able and willing to use it.
Sometimes, a single naloxone dose can save two lives.
In 2018, clinicians in North Carolina treated a pregnant patient who had recently overdosed. Friends had used naloxone to reverse the overdose, allowing her to enter treatment for substance use.
A few months later, she gave birth to a healthy baby.
[ Like what you’ve read? Want more? Sign up for The Conversation’s daily newsletter. ] Screen reader support enabled.![]()
Tarlise Townsend, Joint PhD Student, Health Policy and Sociology, University of Michigan and Freida Blostein, Epidemiological Science PhD Candidate, University of Michigan
This article is republished from The Conversation under a Creative Commons license. Read the original article.