How can all schools safely reopen?
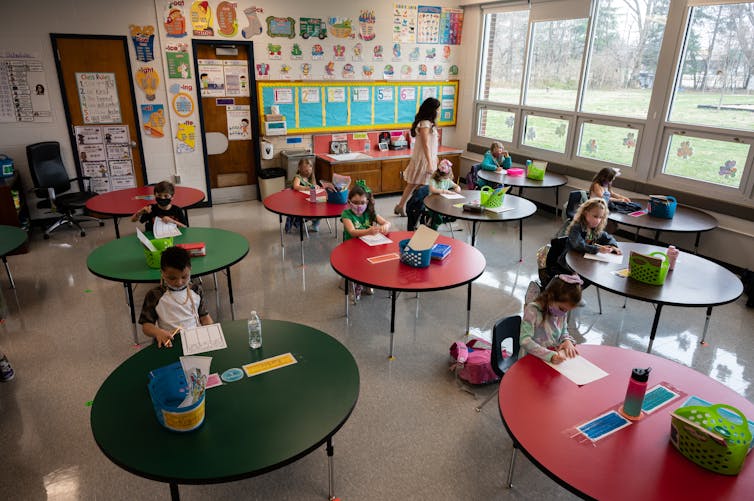
The question of when and how to open schools for full in-person learning in the midst of the COVID-19 pandemic is one of the most consequential the U.S. currently faces. A wealth of evidence suggests that schools can provide in-person instruction with a very low level of risk when safety protocols are successfully implemented.
So, what do school districts, teachers, families and students need to know? As an infectious disease epidemiologist with more than 15 years of research experience – and as co-editor of the COVID-19 Literature Situation Report, which produces a daily summary of the most relevant newly published and pre-print literature related to COVID-19 - I offer answers to some of the most urgent questions about how schools can safely resume in-person instruction. Some of this evidence is gleaned from preprint studies that may change after they are peer-reviewed.
Will school make children more likely to transmit COVID-19?
Infection with the COVID-19 virus has been less common in school-age children, especially those in elementary school, than among other age groups. Evidence from Florida, Utah, Missouri and elsewhere indicates that less than 1% of school-age children have had COVID-19, despite most being in school in person. Most cases have not been linked to school exposures.
While school outbreaks have occurred, most have been small in scale. Transmission from an infected student to others in the household or community has been rare.
While not definitively proved by scientific studies, indications are that elementary school-age children are less likely than older children and adults to transmit the COVID-19 virus to others.
What about teacher and staff vaccinations?

Spread of COVID-19 through in-person K-12 schooling has been limited, even without vaccinations. Teachers are now eligible to be vaccinated in all states in the U.S., which means that the risk to teachers and staff who are vaccinated, as well as to students and others who may not be willing or able to be vaccinated, is greatly reduced. No studies give us a magic number for the proportion of teachers and staff who need to be vaccinated before in-person learning can be implemented. In fact, the Centers for Disease Control and Prevention advises that in-person learning can start safely as long as other mitigation protocols like mask-wearing and adequate ventilation are in place. Vaccines offer an added level of protection.
The vaccines currently approved for use in the U.S. under emergency use authorization are all highly effective at preventing mild, moderate and severe COVID-19 disease, and they also prevent infections.
This means that these vaccines both protect the vaccinated person and reduce the risk of transmission from a vaccinated to an unvaccinated person. This is critical, because at this time there are no vaccines approved for use in those under the age of 16 in the U.S.
Pfizer and Moderna have trials underway in adolescents and hope to have results by late spring or early summer. In the meantime, to protect students from infection, it will help to vaccinate as many adults as possible in schools.
Transmission is far more common from teacher to student and teacher to teacher than from student to teacher. So far, research that has not yet been peer-reviewed shows that the vaccines approved for use in the U.S. have similar efficacy against the newly emerging variants of concern, especially in terms of preventing severe disease.

What is the right amount of physical distancing?
So long as people are wearing masks, there is no evidence that 6-foot physical distancing between students is more effective than 3-foot distancing. This led the CDC to shift its guidance to recommend a physical distancing of only 3 feet in classrooms. Three-foot distancing allows for much more flexibility in terms of classroom size and layout. Face masks are highly effective in reducing infection and transmission risk and are therefore a critical mitigation measure.
In addition, early research suggests that keeping students in groups, or cohorts, and limiting contact among cohorts may reduce the potential for widespread transmission if a case occurs in a school. Cohorting can also minimize the number of students who would need to be quarantined.
On the bus or other transportation
Just as in the classroom, masks work when transporting students to and from school. Double-masking is probably best, especially in indoor spaces, including cars and buses. Ventilation with outside air – either by opening windows or avoiding ventilation that recirculates air – may help to reduce the risk of transmission in buses. Students should space out as much as possible, given the elevated risk of transmission seen among passengers sitting close to an infected individual on airplanes, although universal mask usage is likely to reduce the importance of physical spacing.
While droplet and airborne transmission of the COVID-19 virus appear to be the dominant modes of transmission, hand-washing and using hand sanitizers before entering buses and upon exit may help reduce the risk of transmission through contact with contaminated surfaces.
The gym, recess and after-school sports
Growing evidence shows that kids can play sports and have recess if they are outdoors and players have no or low contact. Based on studies, including some that have not yet been peer-reviewed, activities such as soccer, tennis and cross-country are fine.
The American Academy of Pediatrics recommends that athletes participating in indoor sports wear masks, except those participating in swimming and diving, cheerleading, gymnastics and wrestling, to prevent choking or suffocation. Some indoor sports, particularly wrestling and hockey, have been associated with large outbreaks. Also, outbreaks of COVID-19 have been associated with football teams.
An important finding from a number of investigations is that many of the cases of transmission, including on football teams, appear to be linked to activities not directly related to the sport itself, such as meetings in enclosed spaces without masks, eating together and parties and social events.
Are masks still required?

Masks are likely to be a critical part of protocols to prevent COVID-19 in schools, at least until vaccines are universally available, including for children. Even then, the potential emergence of new variants that are resistant to existing vaccines may make mask usage a necessity for some time. Schools that have provided in-person instruction during the COVID-19 pandemic, including during periods of high community transmission, have experienced few widespread outbreaks directly related to school transmission when masks are used.
This has been true in Florida, Massachusetts, Salt Lake City, England and elsewhere.
In contrast, not wearing masks was a problem in schools in Sweden. In this Scandinavian country, younger secondary-school students returned to full-time, in-person learning without masks and with few other mitigation measures. Older secondary-school students continued with remote learning. Students and staff who went to school in person and without masks or other safety measures had a somewhat higher likelihood of having COVID-19 compared with those learning remotely, although the absolute risk was still quite low.
How critical is soap or hand sanitizer?
While the coronavirus that causes COVID-19 has been detected on surfaces, touching those surfaces doesn’t appear to be the dominant route of transmission. Even so, hand-washing and using hand sanitizers are still good ideas. Face masks and physical distancing are more important, though.
[Deep knowledge, daily. Sign up for The Conversation’s newsletter.]![]()
Brandon Guthrie, Assistant Professor of Global Health and Epidemiology, University of Washington
This article is republished from The Conversation under a Creative Commons license. Read the original article.